Since the outbreak came to our news in December 2019, COVID-19 has claimed hundreds of thousands of lives. Our saving grace came late in 2020 in the form of a vaccine developed by Pfizer and BioNTech. But this has since been overshadowed by the emergence of new variants of the SARS-CoV-2 virus.
In December, the UK saw a huge rise in cases of COVID-19 in the South-East of England. The outbreak led to much of the region jumping from Tier 2 restrictions to Tier 4 and also led to travel bans and concerns from other countries. The higher transmission rates associated with the outbreak prompted investigations through which new variants of the coronavirus were discovered, with mutations that alter the characteristics of the virus’ spike proteins.
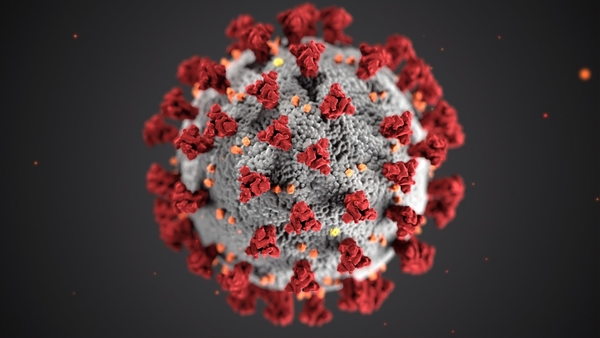
Spike proteins are the proteins present on the outer membrane wall of the virus that help it penetrate host cells.
The UK variant has been spotted in Australia, Denmark, Italy, Iceland and the Netherlands. And there are new concerns of a variant linked to South Africa spotted in the UK.
What does this mean?
All viruses mutate and change, and SARS-CoV-2 is no different. The coronavirus’ characteristics are determined by its RNA (much like how ours is determined by our DNA). This RNA is stored within some nucleocapsid protein for protection, within the walls of its lipid membrane.
The RNA is made up of sequences of nucleotides with the bases: Adenine, Uracil, Cytosine and Guanine. The RNA base sequence codes for sequences of amino acids that make up its proteins. When replicating its RNA for reproduction, often a mutation occurs by chance, and one or more of these bases are deleted, added or substituted leading to a change in its nucleotide base sequence. This can then lead to a changed amino acid sequence and therefore a slightly different protein.
In the case of the variant common in the South-East of England, a mutation in the RNA of the virus led to a change in one of its spike proteins (an amino acid asparagine was replaced with a tyrosine at some position in the protein). The effects of this change haven’t been properly quantified, but if this new spike protein can penetrate host cell walls more easily then the new variant could well be more transmissible.
Is the new variant more dangerous?
All variants of the virus infect us in the same way. The virus is initially inhaled and infects epithelial cells in our nasal cavity and the ciliated cells in our airways. At this stage we’re usually asymptomatic. The virus then replicates down the respiratory tract towards the lungs, at which point we develop the common symptoms such as coughing. Once the virus infiltrates the lungs it can infect our alveolar and lead to shortness of breath and pneumonia.
It’s the spike proteins that are allowing the virus to penetrate our cells and infect them. The spike protein is made up of two subunits. One will allow it to bind to the host cells and the other will fuse the virus to the host cell so that it can inject its RNA. Once the virus’ RNA is injected, it will use the host cell to replicate and reproduce.
If the spike protein changes and it becomes easier to penetrate host cells, it might be more transmissible and infectious. Initial estimations suggested that the new variant was 70% more transmissible. There isn’t any evidence to suggest that it’s any more dangerous or severe to us and PCR tests can be altered and adapted to pick up the new variant.
What do the variants mean for the vaccine?
The new vaccine produced by Pfizer and BioNTech is an mRNA vaccine. This is a relatively new type of vaccine that uses mRNA to tell cells in our body to produce a harmless version of the spike protein. Our body then produces an immune response and antibodies to this spike protein. This will lead to a powerful immune response to the spike proteins on the SARS-CoV-2 virus.
For variants of SARS-CoV-2 to be resistant to our vaccine-induced response, it would need to have mutated significantly so that the spike protein can’t be recognised by our immune system. There is currently no evidence to support this, but it would be concerning. That being said, given that we already have a vaccine for one variant, it would be much easier to produce vaccines for new variants. Think of the flu vaccine; each year a new flu vaccine is produced and distributed because of so much change and mutation within the influenza virus.
We can expect the virus to continue to mutate and change. Given that it has spread all over the world, the virus isn’t going to just leave the population, even once we’re all vaccinated. The first flu pandemic we know of was in 1918, and since then the flu virus has remained in the global population and mutated continuously.
Sign up to recieve our newsletters
Don't miss out on our latest content!
Recent posts
Pramod Kumar | 2022-03-04
How Are Investments in Genomics Driving Research Projects?
Science, Healthcare, Business | 4 min read

Dillon Lad | 2021-07-10
4 ways we're destroying the environment without even realising
Environment | 4 min read

Dillon Lad | 2021-04-26
The science behind The Matrix: can we power the world with our own mind and bodies?
Technology, Science, Film | 4 min read

Dillon Lad | 2021-01-29
Breaking up Big Tech with a decentralised internet for the future
Technology | 4 min read

Dillon Lad | 2020-11-30
The shocking behavioural psychology and design behind the world's social media addiction
Technology, Healthcare | 4 min read